Information about COVID-19 Coronavirus
COVID-19 Testing is at 10am at CWFM- Conroe Location Only
Our Safe Diagnosis Procedure:
•All patients who want to schedule an appointment are screened with the risk assessment.
•If they screen positive, they are urged to stay at home and then are contacted by one of their health care professionals.
•If negative, they are scheduled for an appointment.
•Patients who come to the clinic instead of calling in are screened at the front desk with the same risk assessment, and if the risk assessment is negative, they are scheduled to see a provider.
•If the risk assessment is positive, they are placed in a designated room where they are evaluated by a provider who has all the personal protective equipment needed to appropriately evaluate that patient.
•If the evaluation leads to another reasonable cause for their symptoms, they are treated appropriately.
•If no other cause is identified and they have no life-threatening symptoms, they are educated on how to quarantine at home. (This is important: quarantine means they don’t leave the house. That’s not an easy concept for most Americans to take seriously.)
•If they have life-threatening symptoms, they are sent to the emergency room, and the emergency room is alerted to their impending arrival.
“You just heard exactly what every family doctor needs to have in place in this state, which is how to make sure people who are sick don’t come to their office and that those who come to their office and are sick are triaged quickly and appropriately.”
Insurance & Payment Information
RAPID COVID-19/FLU Testing:
- Rapid COVID tests will now be billed under insurance (except BCBS HealthSelect, Humana, and BCBS TRS HMO)
- Self-pay- $150 new patient or $100 existing patient (no office visit required)
- Every patient will have a telehealth visit and be added to the swab schedule (unless the patient is traveling, repeating a rapid or visiting family in a nursing home or healthcare facility they will not need a visit)
- If a patient has insurance that we DO NOT take they will be required to pay cash for the rapid test, or we can offer them the PCR send out with Alliance.
PCR/ALLIANCE TEST WILL STILL NEED A TELEHEALTH VISIT AND BE BILLED TO INSURANCE. IF THE PATIENT IS SELF PAY WE WILL SEND TO QUEST.
COVID-19 Coronavirus Patient Self-Assessment Tool
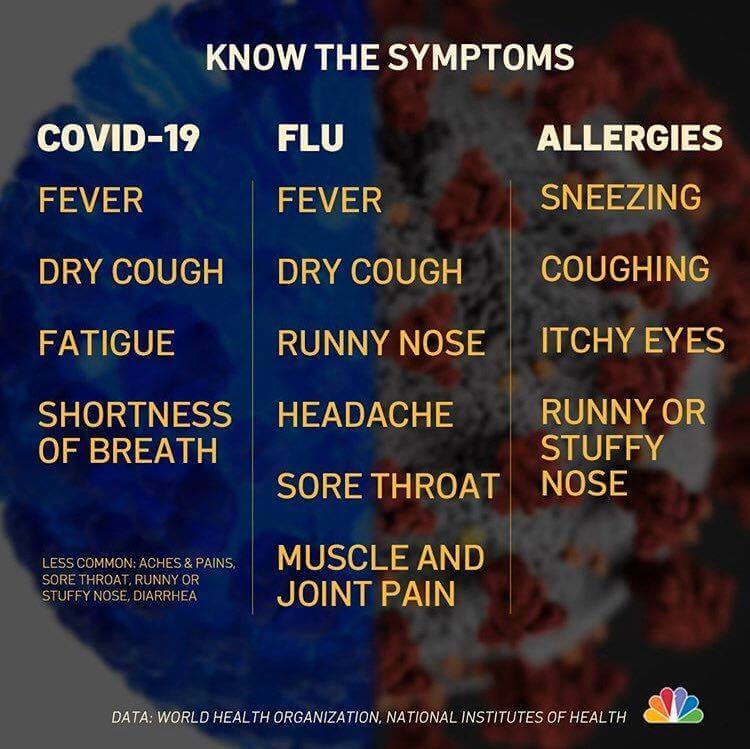
If you have symptoms of respiratory illness (e.g., fever, cough and/or shortness of breath), answer the following questions:
1. Have you recently traveled outside the country? Current countries at high risk include all Asian countries, Italy, and Iran.
2. Have you been in close contact with anyone known or suspected to have the COVID-19 coronavirus illness? Close contact is defined as within 6 feet for 3 minutes or more.
If you answered yes to one or both of these questions and have respiratory symptoms:
•Stay home and call Conroe Willis Family Medicine. A patient representative will take your information and have a health care provider contact you to discuss next steps.
•If you believe your symptoms are life threatening, go to the nearest hospital emergency department. We recommended that you call the emergency department immediately so the staff can provide you with arrival instructions.
•If you do not have respiratory illness symptoms, please refer to information below or contact your local health department.
Quarantine Information
With coronavirus (COVID-19) dominating the news cycle, you’re starting to throw around words like “quarantine” with an uneasy casualness. But what do these words really mean for your life?
“Quarantine doesn’t have to be a scary thing,” explains infectious disease specialist Steven Gordon, MD. “And it’s an effective way to protect the public.”
Dr. Gordon explains the ins and outs of quarantine and other common terms connected with disease outbreaks.
What does quarantine mean?
Governments use quarantines to stop the spread of contagious diseases. Quarantines are for people or groups who don’t have symptoms but were exposed to the sickness. A quarantine keeps them away from others so they don’t unknowingly infect anyone.
Quarantines may be used during:
- Outbreaks: When there’s a sudden rise in the number of cases of a disease.
- Epidemics: Similar to outbreaks, but generally considered larger and more widespread.
- Pandemics: Larger than epidemics, generally global in nature and affect more people.
What’s the difference between isolation and quarantine?
While isolation serves the same purpose as quarantine, it’s reserved for those who are already sick. It keeps infected people away from healthy people to prevent the sickness from spreading.
Can you be legally quarantined?
According to the U.S. Constitution, yes. The federal government can use isolation and quarantine to protect people from contagious diseases. States also have the authority to institute isolations or quarantines. Breaking a quarantine has consequences that range from a fine to imprisonment.
But government-mandated quarantines are rare. You have to go all the way back to the infamous Spanish flu pandemic of 1918-1919 for the last enforced, large-scale isolation and quarantine, according to the U.S. Centers for Disease Control and Prevention (CDC).
In response to suspected or confirmed coronavirus exposure, some have been asked to self-quarantine. And while it’s highly recommended that you do, these quarantines are currently voluntary.
“For anyone who has close contact with someone infected with the coronavirus, it is important that you listen to instructions from your health department,” Dr. Gordon says.
What exactly is “close contact?” It’s defined as being within approximately 6 feet (2 meters) of someone with COVID-19 for a prolonged period of time. That includes if you are living with, visiting or sharing a healthcare waiting area or room with someone with COVID-19. Or if you have been coughed on by someone with the disease.
Health departments identify close contacts through what’s called contact tracing, Dr. Gordon explains. “They will notify you if they think you have been exposed to a known case and provide you with instructions for next steps,” he says. Unsure if you qualify as having been in close contact? Reach out to your local health department.
What happens when you are quarantined?
While not all quarantines are the same, look to the CDC for how best to do your part. Currently, the CDC recommends:
- Make it a staycation: Avoid leaving the house unless absolutely necessary (read: visiting your healthcare provider, though see the next bullet for how to do that). That means no work, school or church.
- Call ahead: While your local or state health department will most likely keep tabs on your health, you may need to see your doctor, too. “First, try a phone visit. Or at least, call ahead first, so that the medical facility can take steps to prevent others from getting infected,” says Dr. Gordon.
- Worried about Fido? At this time, the CDC says there’s no evidence that companion animals, including pets, can spread COVID-19. But it may still be good to still use caution. If you’ve been exposed to COVID-19, avoid “petting, snuggling, being kissed or licked and sharing food [during a coronavirus quarantine],” recommends the CDC.
- Have your own stuff: Don’t swap unwashed “dishes, drinking glasses, cups, eating utensils, towels or bedding with other people or pets in your home,” says the CDC.
- Wash, rinse, repeat: “Hygiene is an integral part of this, even at home. Handwashing should be your first line of defense when under quarantine,” relates Dr. Gordon. “And don’t forget to cough or sneeze into your elbows or a tissue that you then throw away.”
Other protective measures
Quarantine isn’t the only way to protect yourself during an epidemic. Dr. Gordon also recommends:
- Social distancing: Social distancing involves avoiding large gatherings. If you have to be around people, keep 6 feet (2 meters) between you when possible. “Social distancing is pretty much like using common sense,” Dr. Gordon says. “We don’t realize how interconnected we are until we’re asked to avoid people.” But he notes that terms like “mass gatherings” or “congregate settings” are vague. They’re used to describe things like shopping centers, movie theaters or stadiums. But how many people together is too many? “That’s a moving target,” he says. “While the number 25 is often cited, there’s currently no official definition — and that may be subject to change.”
- Staying calm: “While fear is normal, educating yourself is a great way to counterbalance your anxiety,” says Dr. Gordon. “Stay informed from reliable sources — but not too intensely. Hyper-fixating on the news can be just as detrimental.”
- Cooperating with the authorities: Following quarantines and other public health mandates help slow — and stop — the spread of contagious diseases.
Being cooped up inside may seem unbearable. But the time WILL pass, and your forced staycation may save lives.
Currently, coronavirus/COVID-19 has been detected in over 60 countries. Secretary of Health and Human Services Alex Azar reported on Sunday, March 1 that there were 23 cases in the United States not associated with the repatriation of American citizens from overseas. He stated that more cases in additional states are likely. States with confirmed COVID-19 cases include Washington, Oregon, California, Arizona, Wisconsin, Illinois, New York and Massachusetts. The first reported COVID-19 death in the United States was reported in the state of Washington on Sunday, March 1.
Face masks for the general public are not recommended. American Surgeon General, Jerome Adams, has shared that face masks are not effective in the prevention of COVID-19. In fact, the purchase of face masks by the general public is creating a shortage for those most in need: healthcare workers caring for patients with known or suspected infection. The government has now contracted 3M to produce an additional 30 million face masks per month to meet growing use.
- For the general American public, who are unlikely to be exposed to this virus at this time, the immediate health risk from COVID-19 is considered low.
- People in communities where the virus that causes COVID-19 has been reported are at elevated, though still relatively low, risk of exposure.
- Healthcare workers caring for patients with COVID-19 are at elevated risk of exposure.
- Close contacts of persons with COVID-19 also at elevated risk of exposure.
- Travelers returning from affected international locations where community spread is occurring are at elevated risk of exposure.
CDC has issued guidance to help with risk assessment and management of people with potential exposures to COVID-19.
COVID-19 is a new variant of a common family of viruses called coronaviruses. These viruses typically cause respiratory tract infections ranging from the common cold to more serious illnesses like severe acute respiratory syndrome (SARS). Though most commonly found in animals like cattle, cats and bats, some coronaviruses can infect and spread between humans, such as COVID-19 and SARS.
Just like the flu, the coronavirus is spread through coughing, sneezing and close personal contact with other people.
Symptoms related to COVID-19 coronavirus infection range from mild to severe respiratory symptoms. Most patients have fever, cough and body aches. In more severe infections, symptoms may include shortness of breath and/or pneumonia. Symptoms typically appear between two and 14 days after exposure to an infected person.
The risk to you remains very low. Those at highest risk have recently travelled to countries including China and South Korea, followed by Iran, Italy and Japan. People who have had close personal contact with travelers to these countries who now exhibit respiratory symptoms are also at a higher risk. At this point, you are at far greater risk of contracting the flu (get your flu shot today; it is not too late), which in 2018-2019 led to 34,000 deaths in the U.S.
The COVID-19 coronavirus risk should be managed like other potential disruptions to your daily activities: prepare for the worst and hope for the best. Make sure you have at least a two-week supply of critical medications and supplies necessary for good hygiene.
There are currently no medications or vaccines approved for the treatment of COVID-19. A National Institute of Health (NIH) randomized and controlled clinical trial of a medication for patients hospitalized with COVID-19 in the U.S. was recently approved by the Food and Drug Administration (FDA), but is not available to the public. In the absence of a vaccine or medication, good hygiene practices remain the primary method to address wide-spread transmission and supportive care remains the only medical treatment.
The Center for Disease Control (CDC) and the World Health Organization (WHO) recommend avoiding travel to China and practicing good hygiene in the same way you would protect yourself against the flu:
- Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitizer.
- Avoid touching your eyes, nose and mouth.
- Avoid close contact with people who are sick.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue and then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces.
The CDC urges travelers to avoid all non-essential travel to China. The U.S. Department of State has issued a Level 4 Travel Advisory asking people not to travel to China due to the COVID-19 coronavirus outbreak. If you must travel to China, the CDC recommends protecting yourself by doing the following:
- Avoid contact with sick people.
- Discuss travel to China with your healthcare provider. Older adults and travelers with underlying health issues may be at risk for more severe disease.
- Avoid animals (live or dead), animal markets and products that come from animals (such as uncooked meat).
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom and before eating, as well as after coughing, sneezing or blowing your nose. If soap and water are not readily available, you can use an alcohol-based hand sanitizer that contains at least 60% alcohol. Always wash hands with soap and water if your hands are visibly dirty.
As more information becomes available it will be posted on this website. Additional information is available at cdc.gov/coronavirus.